Voices in Humanism Essential Stories
“Good Morning, My Name is Maurice”
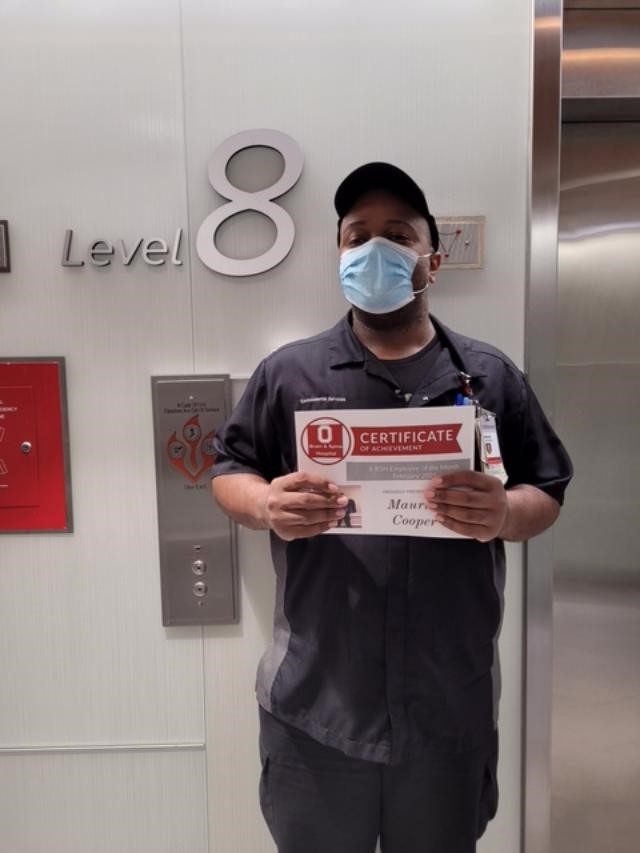
Maurice Cooper, Environmental Services, EVS, The Brain and Spine Hospital, The Ohio State University Wexner Medical Center
Maurice Cooper came into his third year working in hospital environmental services in March 2020 with the same trepidation as most. COVID patients began arriving, and with discoveries yet to be made about this new virus, fears ran high.
“I was worried every single day in the beginning,” Maurice said. “I still get worried about catching COVID and I have been exposed twice and tested twice but I am fine. We learned how to handle cleaning and how to take precautions and that has helped.”
We see news stories of pots and pans being banged to honor doctors and nurses for their selfless work and pizzas delivered to Emergency Rooms to reward the staff. Yet, on the very front lines of infection fighting are our unsung heroes, the housekeeping battalions fighting the sanitizing wars. Without them, the enemy would run rampant defeating all other efforts.
“We go through a three-step cleaning process,” Maurice explained. It consists of first the general clean up, then the thorough clean, and then with the patient still in residence, finding out what the patient also needs to have completed. With a patient diagnosed with COVID and released, there is a thorough bleaching of everything. According to Maurice, this cleaning is welcomed for what it does for the next patient but, “it is also what helps keep us out of the hospital beds too,” he reasoned.
For the COVID patients, Maurice and his co-workers are covered with protective wear head to foot and sometimes he finds it hard to breathe with so much outer wear. None of this prevents Maurice from following protocol and also being a kind human being to even the sickest non-communicative patients.
“Last week I witnessed a death. It was heartbreaking. The person could barely talk. It was a thumbs up or an eye blink,” he related. I would offer my message on the board and write, Good Morning, My Name is Maurice, I am here to clean your room.” Even though the patient lost the battle against COVID, Maurice’s compassion, warm smiling eyes, and cleaning skills showed the patient he and others were there to help.
Consider “sterile” conditions in 1900 hospitals and see how far we have come. Surgeons wore street clothes and shoes with a type of butcher’s apron over top. Open air operating rooms had come-as-you are spectators. Until the 1980’s nurses sported a small white starched cap perched atop their heads. Ambulances were horse drawn carriages. Sanitation improved but 2020’s COVID whirled all into another galaxy of clean.
Maurice recently won “Employee of the Month” on his floor, a recognition he is especially proud of. “I understand usually nurses win the award and the nurse manager said I was the first housekeeper to win it. It’s hanging on the door where we clock in.” Maurice has much respect for the nurses whom he says so often represent the family members who cannot visit the COVID patients and do an incredible amount of work under extreme circumstances.
Director of Environmental Services at Ross Heart Hospital, Meghan Taucher, said of Maurice, he is someone you can rely on. “He goes out of his way to help anyone and everyone. He has the biggest heart and is one of the kindest people I have ever met. Maurice cares so much about his job. He knows how important his role is in keeping the patients and staff members safe. He works hard day in and day out but always does so with a smile on his face. You can tell that he loves what he does and loves making a difference in people’s lives. Maurice is AWESOME!”
Maurice’s respect for others extends to his managers and the hospital system itself. He said with a crack of emotion in his voice, “I am so touched by what Meghan said about me. She goes out of her way to be understanding. You know, that patient in the bed could be any one of us in the hospital and that’s why I do my work the way I do. I try and set a good example with my job and pass it on to others.”
Manager Brice Hulsether also receives high praise from Maurice for making sure they have everything they need to sanitize and maintain cleanliness; priority one in a hospital. As far as working for the hospital, Buckeye fan Maurice Cooper feels about his work environment as he does about next year’s OSU football team. He said, “I have faith in them.” He also said, “The entire hospital, everybody inspires me in their own way.”
Maurice’s work ethic is heaven sent. “Just make the best out of everyday and bring all the smiles. Do what you’re supposed to do and do not worry about what you cannot do.” Those are the words of Maurice’s mother who instructed him in how to be a good person. His mother passed away at the age of 48. Maurice, now 35, said, “Her words stick with me every day.” His mother cautioned, “You can’t do everything. Do what you can.”
In the height of the pandemic when everyone needed to acknowledge what they could do and what they could not do, that dark cloud of helpless stress fell heavily throughout the hospital among dedicated individuals who are trained to nurture, heal, and save. COVID was testing their resolve. Still, everyone soldiered on, masked, with hands cracking from so many washings. They set aside sadness and fear in order to treat and save patients.
Not everyone could be saved, but everyone can follow Maurice’s mother’s advice and do what they can and “bring the smiles” while they work.
Sometimes a glorious saving grace could be a face of sincere warmth, even masked, and words of care written on the board: “Good Morning, My name is Maurice. I am here to clean your room.”
With Maurice and all of the housekeepers, the old adage is true, cleanliness is next to godliness.
Patricia Wynn Brown
Writer and Performer
Medicine and the Arts Board
Author: ESSENTIAL STORIES: Medicine During Covid-19 and the Lives of the Practitioners at The OSU Wexner Center





















Recent Comments